 The role of insulin resistance and cholesterol. The truth about cholesterol.
The role of insulin resistance and cholesterol. The truth about cholesterol.
Let’s first start with the truth. Cholesterol is not the problem with heart disease, insulin resistance and toxicity are. As stated in other articles on this website, insulin resistance is a major indicator of many diseases. Metabolic imbalances need to be corrected in order for insulin resistance to disappear and for cells to heal and live. Insulin resistance can be caused by a number of factors such as skipping meals, eating large quantities of processed and refined foods and drinks, stress, low physical activity levels, and toxic overload.
First, what is cholesterol and why do we have it?
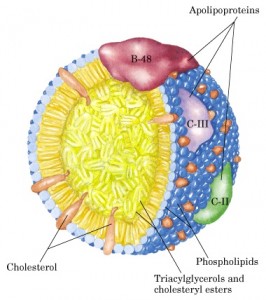
Cholesterol is a waxy substance that travels through the body in the form of lipoproteins known as low density lipoproteins (LDL) and high density lipoproteins (HDL). Most of our cholesterol is in the form of LDL’s. Cholesterol is synthesized in the liver and essential for the transport of fatty acids, cellular structure, hormone production, and the production or synthesis of bile acids and vitamin D. There really is no “bad” cholesterol because both LDL and HDL are important for cellular function and health. HDL is different in the sense it is responsible for bringing LDL cholesterol back to the liver for elimination or to be used in other organs.
What’s the deal with all the hype about high cholesterol?
Scientists used to think that high cholesterol lead to the excessive build up in the arteries leading to atherosclerosis and heart disease. We now know that the bodies release of cholesterol is essential for cellular function, but high cholesterol maybe a response to inflammation and stress. The body is doing what it’s supposed to do when it raises cholesterol. The damage that is done to arteries is not due to cholesterol alone but to excessive oxidative damage from excessive levels of LDL’s in the blood stream as well as metals and other toxins.
What causes LDL levels to rise?
The release of cortisol triggers fat cells and the liver to release fatty acids into the blood stream along with toxins. Toxins are stored in fatty tissue and other connective tissue. Cortisol is triggered by increased insulin levels, such as after a meal and times of stress such as with the fight or flight response. It’s job is to release high energy fatty acids and lipids into the blood stream so cells can utilize this energy quickly, but also for other cellular functions and cell structure.
Unfortunately, we are not living in a time of much fight or flight situations. Our stress is termed, chronic. That means, we have prolonged times in our day where insulin and cortisol levels remain high. The constantly high insulin levels lead to cellular malfunction and inefficiency of energy use. The constantly high levels of cortisol lead to excessive levels of free fatty acids and toxins in the blood stream. Oxidation of these fatty acids become excessive as well. With excessive oxidation, you have excessive free radical damage to cellular structure.
Cholesterol is a major part of cellular structure. As you can see, damage to cellular structure sends signals from the cells to repair this structure. Unfortunately, weakened cellular structure causes a host of other imbalances inside the cell. Calcium and sodium balance is effected. The damaged cells begin to enlarge with calcium deposits and swell. Cholesterol is only trying to do it’s job by repairing the structure of the cell. The arterial wall becomes hard due to the calcification, not the cholesterol. As this continues, the arterial walls become more and more inflamed, calcified and higher amounts of cholesterol repair leads to the closing of the arterial wall which leads to the slowing of blood flow and high blood pressure. This increases risk of heart disease and stroke.
Oxidation is unavoidable and part of our immunity, which is very helpful. As with many things that become out of balance, there is disruption. In this case the disruption can be very damaging and increase risk for disease and illness. One would think that higher levels of HDL would correct this problem because it’s responsible for “clearing out” LDL’s. Unfortunately, the increase or excessive amounts of triglycerides from insulin resistance and high cortisol levels causes and increase in LDL and this mechanism stimulates enzymes that lower HDL. The more LDL, the more oxidation and oxidative damage.
Basically, the only way the body can get cholesterol, triglycerides and phospholipids to the cells is through the transport of these lipoproteins. As the body takes what it needs, the lipoproteins become smaller. The molecular make up of LDL’s become highly oxidative, mostly because it’s lost it’s protective substances. HDL is responsible for taking these LDL’s back to the liver to recapsulate more cholesterol, triglycerides, and phospholipids to go back out into the body for normal cellular function. Triglycerides are simply another high energy fat that are released in times of high insulin, high blood sugar, and high cortisol. The higher the triglycerides, the more LDL cholesterol you need to make in order to transport it through the body for use or excretion. Toxins also increase oxidation and damage cells.
Cortisol is also responsible for the breakdown of muscle which leads to loss of protein stores. The reason cortisol breaks down muscle, and other connective tissue, is for the use of certain amino acids for gluconeogenesis, the creation of glucose for normal metabolic functions. Loss of muscle or metabolic tissue can put you at greater risk for disease and illness.
There are things we can do to correct these imbalances.
Eating foods high in antioxidants, eating regularly scheduled meals/snacks, getting daily exercise, proper sleep habits, avoiding toxins, and of course reducing stress. Skipping meals, eating erratically, not getting enough sleep or exercise are all forms of stress. Add psychological worry, fear, sadness, and anxiety and you are looking at a life of ailments and poor quality health. (See our page under Mind Body Spirit for stress management tools.)
Another factor that may require additional support would be the genetic inability to detoxify properly. Some people genetically have poor signalling that needs to be corrected with specific supplements. An example would be someone who is deficient in their methylation pathways. For example, a person can be an “over” or “under” methylator and require “support” in order to complete or regulate pathways in the body. Many who turn to pharmaceuticals are unaware that adjustments to diet, intestinal health and specific nutrients can help correct their diseases. The study of epigenetics has provided enlightening information that can greatly improve your health. Food is your medicine.
To learn more about how you can reduce your heart disease risk, schedule your free 15 minute initial consultation today.



 Providing nutritional therapy and lifestyle education for disease prevention and weight management....
Providing nutritional therapy and lifestyle education for disease prevention and weight management....